Green light for osseointegration in Norway

Osseointegration was invented in Gothenburg in the early 80’s. Today, Rikshospitalet has been given the green light to carry out the treatment in Norway. They will operate on the very first patients with good expertise from Gothenburg in Sweden already in December and from the new year. The orthopedists at Rikshospitalet are looking forward to […]
The orthopedists at Rikshospitalet are looking forward to the very first treatments of osseointegration for prosthesis users.
By Marte Nordahl.
Magne Røkkum, Head of Department and Professor at the Department of Orthopedics at Rikshospitalet, is responsible for all treatment of Villy Andresen. Magne has worked as an orthopedist at Crown Princess Märtha’s institute and Rikshospitalet since 1985.
– It will be very exciting to be part of the orthopedic procedure. The new treatment method has been in use for many years abroad, especially in Gothenburg. Only now have we received permission from the state to offer osseointegration in Norway. Here at Rikshospitalet, we will follow up these patients systematically to see how they are doing, says Magne Røkkum.
An expensive methodology
Magne informs that they have planned to operate on the very first patients only at the turn of the year. They are now working to gather suitable patients for this operation.
– We have already started to evaluate some patients, and Villy Andresen is one of them.
We will receive assistance from our friends in Gothenburg with the first operations, so we are absolutely sure that they will be performed in an optimal way, he says.
– So far, there are probably many patients in the country who could benefit from an osseointegrated prosthesis, but who have not received the offer. Only a limited number of patients have been granted permission to perform the treatment in Gothenburg at the expense of the Norwegian state. That the treatment is expensive is a bit of the reason why we have now received permission to perform this in Norway. Carrying out the treatment here in Norway will be significantly cheaper than in Sweden. In addition, it becomes less stressful for the patient.
Old Swedish technology
-
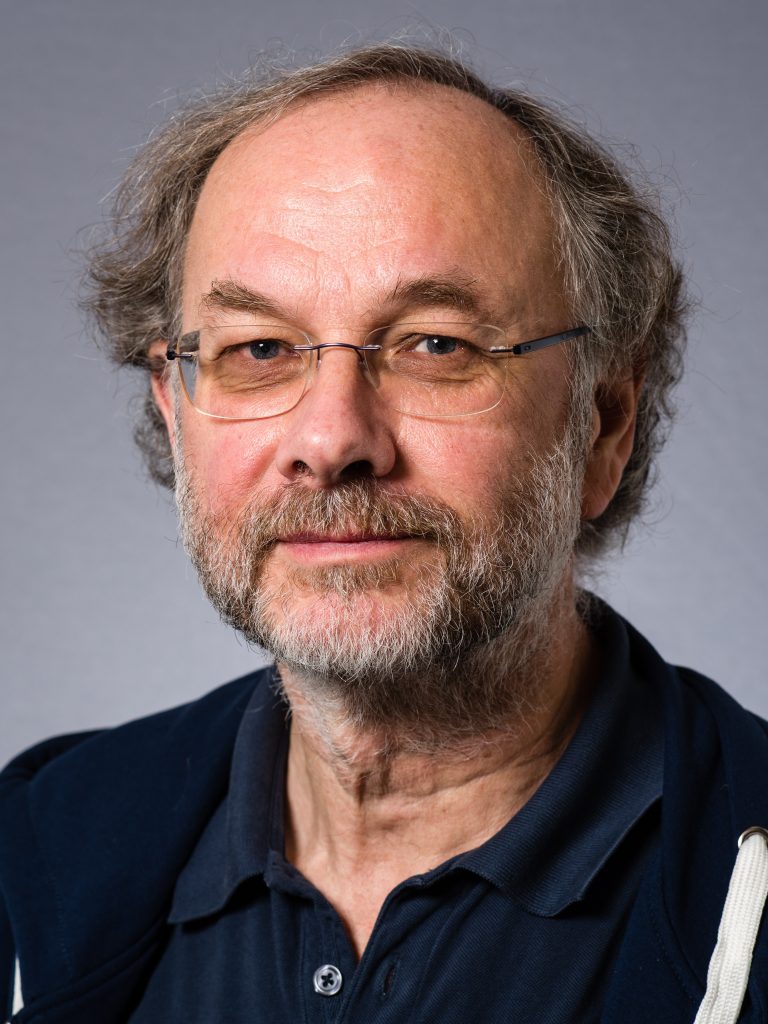
Associate Professor – Department of Orthopedics. Photo. Øystein Horgmo / UiO -
-

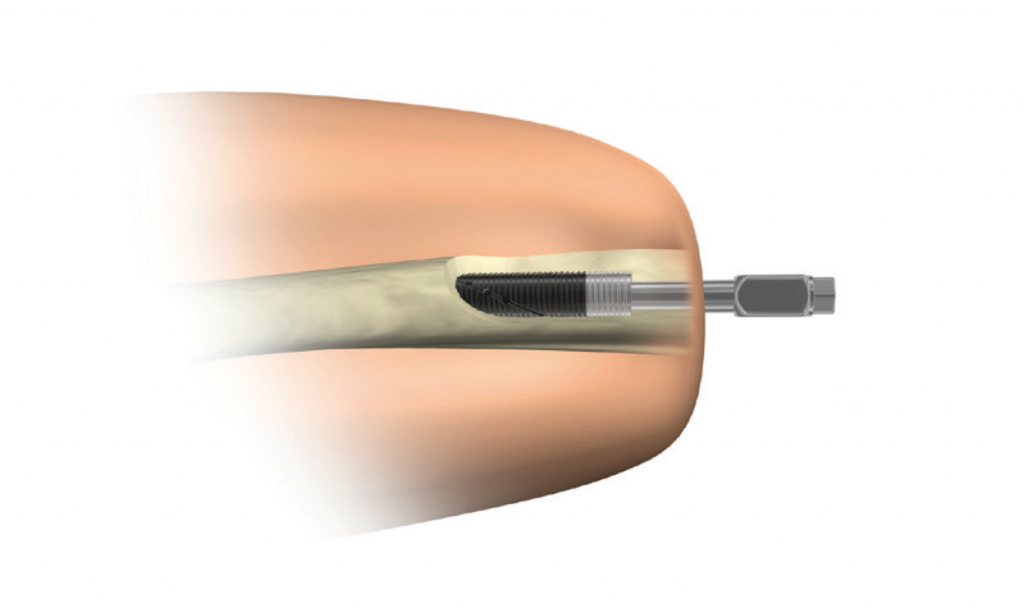
A bolt is screwed into the medullary canal on the leg of the amputation stump. Then the skin and soft tissues are closed again. After a while, a new bolt is inserted that goes out through the skin
Magne highlights the competent research environment in Gothenburg as the heads behind osseointegration as a method, which was discovered in the 80s.
– I got to know the environment myself while I took my doctorate many years ago. The researchers found that if they screwed titanium into the skeleton, it grew firmly without the formation of a connective tissue membrane between the metal and the bone, he informs.
He highlights the well-known method called «Swedish teeth», which has become big business. Titanium screws are screwed in and should sit for 3-6 months, until it attaches well. Then fasten teeth on top of the screws. This method is also used for osseointegration of prostheses.
Operates into the skeleton
– We start with an operation where we screw a bolt into the medullary canal on the leg in the amputation stump. Then the skin and soft tissues are closed again. After a while, a new bolt is inserted that goes out through the skin. When the area is healed and ready, it is connected to a traditional prosthesis. The prosthesis is then attached directly to the skeleton through the bolt that is inserted, he explains.
– Only after 3-6 months will the bolt in the bone grow tight. You will gradually be able to load the leg and apply the new prosthesis over time. Normally it will take about a year until you get permission to load the leg without restrictions. (In the meantime, you can use a regular prosthesis), Magne informs.
Short amputation pieces
Magne emphasizes that osseointegration is most suitable for patients with short amputation stumps. With a short stump, it can be challenging to wear a regular sleeve.
– The method is also suitable for patients who have problems using traditional prostheses for other reasons. For example, those with scar tissue and a tendency to ulceration. Some patients also have challenges with the amputation stump varying slightly in size, so that the prosthesis can be perceived as too large or too narrow. Some patients also complain of pain and other discomfort when using traditional sleeve prostheses. They can also be helped by such skeletal anchored prostheses, Magne informs.
Femur and upper arm
– An osseointegrated prosthesis is well suited for those with amputated femurs and upper arm. The solution can also be used on legs and forearms. Secondly, there is also a variant that reconstructs the thumb, by screwing a bolt into the rest of the thumb. When the wound has healed, it is mounted on a thumb prosthesis.
Magne elaborates that it is most often users who have been in an accident or developed tumor who choose an osseointegrated prosthesis. The solution can be considered in other cases as well. Even the prostheses are not very relevant for users who have had their leg amputated due to poor circulation or diabetes.
Simple and flexible type of prosthesis
Magne emphasizes that since the bolt is connected directly to their skeleton, the user experiences better control and monitoring of the prosthesis.
– It is also much easier and faster to snap on this prosthesis than a traditional sleeve. Likewise, the prosthesis is placed completely stably on the skeleton. Younger amputees in particular will find that this solution provides many opportunities for activity, he says.
Challenging with infection
– The operation itself is not very difficult. It is, of course, a work that requires accuracy down to the fingertips. But it is not among the most difficult orthopedic surgeries we perform. Both the surgical and technical aspects of the operation are affordable.
– When inserting the bolt, we apply all necessary measures to avoid an infection. It is very rare that it occurs. On the other hand, in the long run, bacteria can creep in between the bolt and the skin. When a metal bolt protrudes through the skin, there will always be a gateway for bacteria. Therefore, very strict hygiene is required. Nevertheless, a significant proportion of patients develop episodes of infection. The vast majority of infections are superficial and can be solved with traditional antibiotic treatment. It is rare that it causes the entire prosthesis to fail. The worst that can happen in that way is that the infection runs into the bone where the bolt is attached. This can be difficult to get rid of. Fortunately, the vast majority of infections are superficial, and which experience has shown to be manageable, he informs.
15-20 patients a year
– In Sweden, they perform around 30-40 prostheses with osseointegration every year. If those numbers are correct, it is conceivable that we will perform around 15-20 patients per year, he informs.
– It will be very exciting to see how the result will be. It is also good to work with something that we believe will benefit the patient. The users we have been in contact with who have had such a prosthesis adapted in Sweden, have been very satisfied with the operation.
– Now we look forward to helping Villy. He is a positive guy, and I have good reason to believe that this will go well. If we also get more current candidates, we are positive to accept them, he says.

